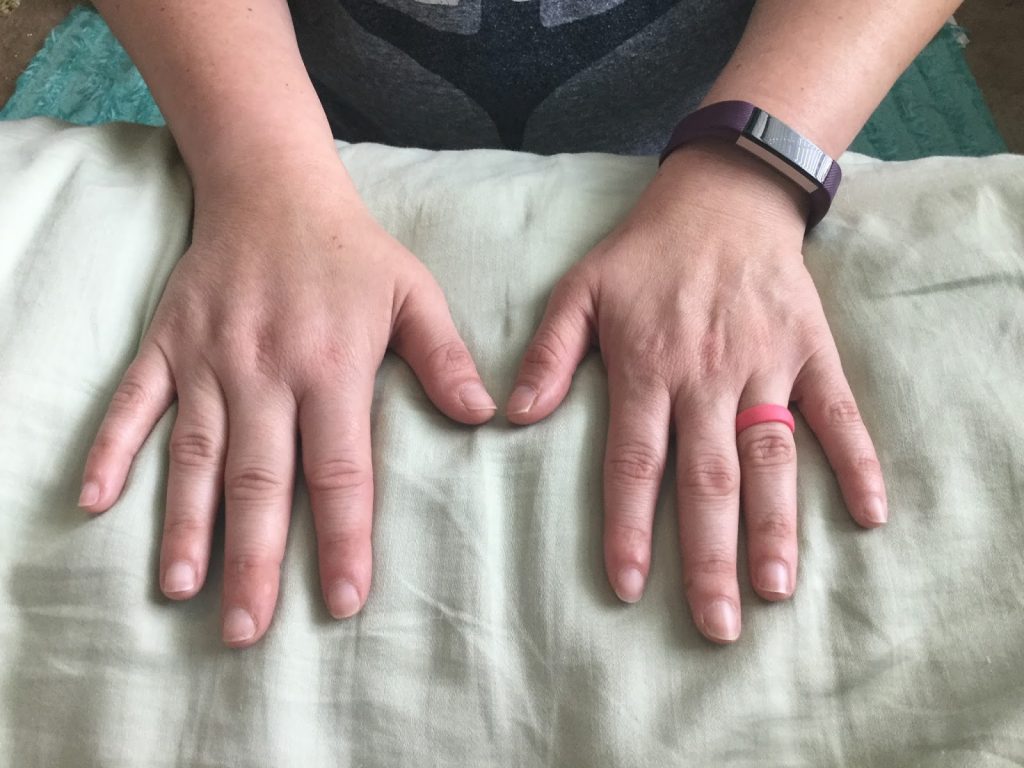
This medical condition is an accumulation of protein rich fluid in the tissues below the skin. This oedema or swelling occurs when lymph fluid cannot drain away. This condition should be treated by a medically trained Clinical Specialist in Lymphoedema
What Is Lymph ?
The lymphatic system is made up of organs such as the tonsils and spleen and a network of nodes and lymph vessels which extends throughout the body.
There is a continuous flow of fluid within our bodies. It passes from the blood in the body tissues and from here into the Lymphatic system. Here the fluid is filtered through the lymph nodes before it is returned to the bloodstream. This constant flow balances the amount of fluid in different parts of the body. When this flow is out of balance, there is a build up of protein rich fluid which is Lymphoedema.
Signs & Symptoms
Some of the signs and symptoms of Lymphoedema include feeling of stiffness in affected areas, slight to severe swelling, sensation of tightness, fullness or heaviness in the affected area.
Lymphoedema manifests itself as a ‘discomfort to aching’ swelling, sometimes it may be painful.
What Causes Lymphoedema?
There are two types of Lymphoedema, Primary and Secondary
Primary Lymphoedema usually happens because the lymph vessels have not developed properly. When there is no obvious cause for Lymphoedema it is generally classed as Primary.
Secondary Lymphoedema is when there is an external cause. It may appear when lymph nodes or vessels have been damaged.
Here are some examples of why Secondary Lymphoedema occurs:
- Cancer or cancer treatment, when lymph nodes are removed or radiotherapy to the lymph nodes
- Any non-cancer related surgery to any part of the body where lymph nodes have been removed or damaged
- Infection of the skin and / or tissues that damage the lymphatics e.g. cellulitis
- Poor blood drainage through veins
- Inability to exercise or move a limb e.g. wheelchair bound
Can Lymphoedema Be Treated?
Lymphoedema is a progressive condition, meaning over time it tends to get worse, but it can be treated and managed. Best results are achieved when treated early. The most successful treatment is Complex Decongestive Therapy (CDT)
Points To Note:
Lisa is a certified clinical specialist in Lymphoedema, trained in both the Dr Vodder and Foeldi methods. If Lisa is not in your local area, a full list of qualified, certified, registered specialists is available on mldireland.com
You can claim for all your treatments via Revenue and Private Health Care.
There are numerous names for this therapy including, Combined Physical Therapy (CPT)Decongestive Lymphatic Therapy (DLT) Complex Decongestive Physiotherapy (CDP)
All of these names describe the same treatment which consists of Two phases, The Intensive phase and the Self Care Phase.
Phase 1, Intensive Phase
- Meticulous skin and nail care to avoid fungal and other types of skin infections such as Cellulitis. The protein rich fluid is an ideal breeding ground for bacteria etc.
- Manual Lymphatic Drainage, this special type of massage moves and redirects lymph flow around affected areas into healthy areas which helps to decongest the area.
- Compression Bandages are used daily, resulting in a dramatic reduction of limb volume.
- Exercise is performed with the bandages in place as bandages improve the efficiency of the muscle and joint pump. Exercises include stretching and diaphragmatic breathing. Exercise increases the lymphatic return, increases lymph vessel activity therefore helps fluid to be absorbed and dealt with by the body.
Phase 2, Self Care Phase
- Compression Garments
- Meticulous skin and nail care to prevent infection
- Exercise daily
- Manual Lymphatic Drainage
- Follow up visits
With damaged or blocked Lymphatic drainage, you are always at risk of infection which could lead to cellulitis in the affected limb, therefore always observe the following
| Avoid | Use |
|---|---|
| Cuts | Gloves when washing up |
| Scratches | Gardening gloves, thimble when sewing |
| Burns | Use oven gloves |
| Sunburn | Complete sun block |
| Insect Bites | Insect repellents |
| Fungal Infection | Good Hygiene and skincare |
| Razors | Depilatory creams |
In Affected Limb / Area
- Never allow anyone to take bloods or give vaccines in affected limb, use the non affected limb as it can easily cause an acute inflammatory process.
- Avoid blood pressure readings on affected limb
- Avoid tight or restrictive clothing or jewellery, especially watches
- Avoid extremes of heat or cold such as saunas, steamrooms or Jacuzzis
Lymphoedema is something that can be well managed.
Additional Indications
One of the cornerstones of treating Lymphoedema is Manual Lymphatic Drainage(MLD). However MLD is a treatment in its own right, focused on other conditions.
There are very few absolute contraindications to Manual Lymphatic Drainage (MLD) therefore it can be used in treatments of many pathologies. It can be used in a potent way to activate the lymphatic system especially when the transport capacity is reduced because of surgery, scar tissue or trauma.
Indications
- Post trauma swelling e.g. sprain, whiplash, hematoma
- Post surgical swelling e.g. facelift, liposuction, breast reduction or augmentation, Joint replacement surgery.
- Fibromyalgia
- Chronic Fatigue Syndrome
- Rheumatoid Arthritis
- Complex Regional Pain Syndrome
- Scleroderma
- Fibrocystic Breast Disease
- Tinnitus
- Migraine / Sinus headaches
- Cellulite
- Palliative care
- Pain Control / General relaxation
- Lipedema
- Detoxification / Enhanced Immune Function